OncoCare
Cancer is commonly construed as a painful condition. Indeed, what many patients, especially those with advanced cancer, fear is unrelenting and intractable cancer pain. It may therefore be a surprise to some that as many as a quarter of patients with advanced cancer do not have a significant pain issue. Moreover, it is also reassuring to note that regardless of the stage of cancer, there are ways to relieve pain, such that no one should tolerate pain or worse, die in pain.
Common causes of pain in cancer patients
There are many causes of pain among cancer patients. These may be:
• Cancer-related
The cancer may cause pain by directly infiltrating and damaging body tissues such as bones, soft tissue, organs and spinal cord. Pain may also arise from distension of the bowels due to intestinal obstruction. When the bone tissues are replaced by cancer cells, severe pain may occur when the weakened bone fractures. Cancer can also compress nerves and cause neuropathic pain.
• Treatment-related
Pain may also be caused by the side effects of treatments such as chemotherapy, immunotherapy, or radiation therapy. Acute pain may occur after invasive procedures or surgery.
• Other causes
Pain may result from complications of prolonged immobility, such as stiffness, contractures and pressure skin sores. Constipation may also be a cause of abdominal or perianal pain.
Apart from physical pain, emotional and psychosocial distress can also present as or aggravate bodily pain and discomfort.
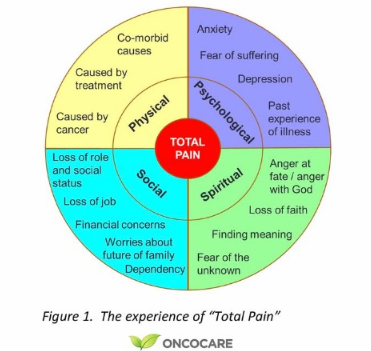
Indeed, pain is often a whole person's experience and teasing apart the different aspects of pain is neither possible nor useful. The term “total pain” has been used to describe such multi-layered and complex pain experiences (Figure 1). An approach that seeks to address all aspects of pain may be needed to provide sustainable pain relief.
The importance of managing pain
Some patients and clinicians still believe that pain is unavoidable and even should be expected in cancer. Others may feel that pain should be tolerated instead of taking more medications since it is a “usual” part of the condition. However, we now know that when pain becomes poorly managed and becomes chronic, changes can occur in the nervous system that make the pain more severe and difficult to treat. Moreover, it is known that patients with poorly controlled pain are more likely to have diminished well-being, more depression and poorer quality of life. There is also evidence that unaddressed pain may hurt survival.
Management of cancer pain
The management of cancer pain begins with identifying the different causes of the pain. Wherever possible, the treatment should be directed at the cause(s) of the pain. This may include different modalities such as treating infections with antibiotics, relieving constipation, surgically removing cancer tumour masses or obstructed bowels, fixing bone fractures, and chemotherapy or radiation therapy for cancer. While treating the cause of the pain or when no options are feasible to deal with the cause of the pain, treatment with analgesic medication (“pain killers”) should be considered.
The World Health Organisation Step Ladder approach is a useful guide for the relief of cancer pain. Those with mild pain may be started with step 1 analgesics such as paracetamol or non-steroidal anti-inflammatory drugs (e.g. aspirin, diclofenac, ibuprofen or etoricoxib). For those with moderately severe pain, one may use weak opioids such as tramadol or codeine. For those suffering from severe cancer pain, it is advisable to commence on strong opioids such as morphine, oxycodone or fentanyl.
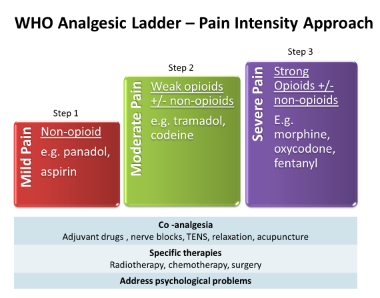
Figure 2. The WHO Analgesic Ladder
At the same time, depending on the mechanism of pain, the addition of adjuvant pain medications may be appropriate. Hence, pain associated with an inflammatory component can benefit from the use of corticosteroids. Pain arising from nerve irritation or compression may also respond to medications such as anticonvulsants (e.g. pregabalin, sodium valproate), or antidepressants (e.g. nortriptyline, mirtazapine, duloxetine), which are known to alleviate pain as well. Adjuvant therapies also include radiation therapy for bone metastases or rapidly expanding cancer masses which are causing pain. Acupuncture, heat or cold therapies, and relaxation are some of the non-pharmacological methods that may be useful for pain relief.
Interventional strategies may be employed in selected cases where the pain is very localised. These include nerve blocks, where injections are guided by imaging scans to numb or destroy the nerves involved in the pain sensation. Fine catheters may also be inserted to deliver focussed doses of pain medications or anaesthetic along the affected nerves as they exit the spinal cord (epidural) or into the space within the spinal cord itself (intrathecal). By focusing directly on the affected nerves, these methods may help to reduce the amount of medication used for pain relief.
With the use of various modalities for pain relief, cancer pain can be controlled in the vast majority of patients. It is important to realise that no patient needs to suffer from severe uncontrolled pain, even if they have advanced or terminal cancer. Yet, there are many times when the patient’s pain remains poorly treated. Apart from the lack of awareness about the availability of cancer pain management, some patients and their families may have opted out of appropriate pain treatments because of various myths about strong painkillers such as morphine. Examples of these include:
Myth #1: Morphine is only for people who are actively dying because it can cause death
- When used appropriately for pain relief, morphine does not hasten death. What often happens to some patients is that they postpone the use of morphine, suffering in pain till they are imminently dying. As a result, by the time morphine is finally used, it is also just before they die.
Myth #2: Morphine is addictive and should be avoided
- When used only for pain relief, morphine does not result in addictive behaviour. If the cause of the pain is addressed and the pain becomes better, there is usually no problem in gradually reducing or eventually stopping the use of morphine.
Myth #3: If we use morphine too early, then there will be no other strong medication left when the pain becomes more severe
- The range of doses for opioids, including morphine is very wide and stepping up the dose can usually meet the needs for pain relief. Moreover, as mentioned earlier, there are many modalities of treatment available so there are many choices apart from morphine. The need to treat pain adequately has been discussed earlier.
Myth #4: Morphine will drug the patient and render the patient incapable of clear mental function
- Morphine may result in drowsiness when used in people whose bodies have not developed the tolerance to opioids, or when the dose has been rapidly increased or when the doses are too high (in the toxic range). It should also be noted that the purpose of pain relief, especially early on in the disease trajectory, is not just to provide comfort but to enable the person to still do what they are capable of when not in pain. Drowsiness can usually be avoided with careful dose adjustments and in fact, many patients can restore their ability to engage in their usual activities when the pain is adequately controlled by morphine.
Site Map | PDPA | Terms of Use | Disclaimer |
Contact Us | Career | Media Contact