OncoCare
Ovarian cancer remains a formidable health challenge globally, striking numerous women with little warning. In Singapore, it's consistently listed among the top ten cancers, with 1,855 cases reported between 2017 and 2021, alongside 12,735 instances of breast cancer, according to the Singapore Cancer Registry Annual Report 2021.
Often, ovarian cancer eludes early detection, typically being diagnosed at advanced stages—III or IV—making effective treatment more complex. The difficulty in spotting early symptoms of ovarian cancer underscores the importance of understanding risk factors and considering preventive measures, especially for those genetically predisposed to the disease, such as BRCA1 mutation carriers.
Among such carriers, proactive steps toward prevention have become a beacon of hope. For instance, the BRCA1 gene mutation not only elevates the risk of breast cancer but is also linked to aggressive forms like triple-negative breast cancer (TNBC), known for its challenging prognosis. This reality has led to high-profile decisions to undertake preventive surgery, famously exemplified by Angelina Jolie in 2015.
After revealing her BRCA1 mutation status, Jolie opted for preventive surgery to remove her ovaries, aiming to mitigate her heightened risk of ovarian and breast cancer, spotlighting a critical question: Should women consider surgery to preempt ovarian cancer?
While no method guarantees complete prevention of ovarian cancer, certain strategies are associated with a reduced risk. Understanding which actions, other than preventative surgery, might lower the risk for ovarian cancer is crucial for women, especially those with genetic predispositions or a family history of the disease.
Simple measures can contribute to lowering the likelihood of developing ovarian cancer. Some of these include:
With these preventive measures in mind, how does surgery play a role in averting ovarian cancer, especially for those at higher risk?
Surgical interventions, specifically designed as preventative measures, can mitigate the risk of ovarian cancer, especially for women at high genetic risk. One of the most definitive preventive strategies is the prophylactic removal of both ovaries and fallopian tubes, known as bilateral salpingo-oophorectomy.
While this surgery significantly decreases the likelihood of developing ovarian cancer, it does not eliminate the risk entirely. In some cases, cancers may already be present at the time of surgery, undetectable until the tissues are examined post-removal. Although the overall risk remains low, this highlights the critical nature of timing and comprehensive evaluation prior to undertaking such preventive surgery.
This raises an important question: if surgical options are available to mitigate risk, what other factors should be considered when deciding on such a profound preventive measure?
Prophylactic surgery, specifically the removal of the ovaries and fallopian tubes, is a critical decision for women at high risk of ovarian cancer. This preventive measure, known as prophylactic oophorectomy, is usually considered for those who have a significant genetic predisposition, such as a BRCA mutation. Several studies have shown a significant (more than 80%) risk reduction in ovarian cancer following risk-reducing oophorectomy.
The importance of this surgery stems from the challenge of detecting ovarian cancer in its early stages. Most cases are diagnosed at an advanced stage. Therefore, by removing both the ovaries and fallopian tubes, women can significantly lower their cancer risk, although it's a decision that comes with its own set of considerations and should be made in consultation with healthcare professionals.
Aside from prophylactic oophorectomy, another surgical option is a hysterectomy—the removal of the uterus. While a hysterectomy does not directly prevent ovarian cancer, it may indirectly reduce the risk when performed for benign reasons. In some cases, the ovaries are left intact during a hysterectomy to maintain hormonal functions and avoid premature menopause. However, retaining the ovaries means that the risk of ovarian cancer, though diminished, remains.
Emerging research suggests that the origins of many ovarian cancers lie in the fallopian tubes. As a result, some women opt to remove their fallopian tubes while preserving their ovaries to lower their cancer risk. For women with heightened risk factors, such as those with BRCA mutations, combining a hysterectomy with the removal of both ovaries and fallopian tubes can significantly decrease their lifetime risk of ovarian cancer.
However, it's crucial to acknowledge that while this reduces the risk considerably, it does not eliminate it entirely. Rarely, peritoneal cancer, which originates from the same cells as ovarian cancer, can still develop. This is why ongoing vigilance and regular medical check-ups remain vital for women who have undergone these procedures.
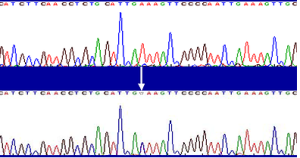
Narrowing in on carriers of cancer-associated mutations, carrying a BRCA mutation significantly influences the likelihood of developing ovarian cancer. In fact, research indicates that about 5.8% of women with the BRCA1 mutation may be diagnosed with ovarian cancer. This statistic brings to light the increased risk that these genetic mutations pose.
While the presence of a BRCA1 or BRCA2 mutation does not guarantee the development of cancer, it does elevate the risk compared to the general population. And despite this heightened risk, it's crucial to recognise that being diagnosed with a BRCA mutation does not change the survival rates for those who develop cancer. However, the knowledge of such a risk can be daunting for most.
So, what treatments are available for ovarian cancer linked to BRCA mutations? Some of the effective options include:
Ovarian cancer is often detected late, typically at stage 3. And inevitably, many wonder why, if the risk for ovarian cancer is heightened, we do not simply rely on regular scans or blood tests for monitoring.
The screening tools available for ovarian cancer, such as transvaginal ultrasound examinations and serum CA 125 concentration tests, unfortunately, have limited effectiveness in detecting the disease early. Plus, these measures have not been proven to lower the mortality rate associated with ovarian cancer. However, for women who opt to postpone preventive surgery, these screening methods are considered part of ongoing preventive strategies. The CA-125 test, which detects a protein that can be a marker of cancer, is convenient to administer but can also show elevated levels due to benign conditions.
Some questions about preventive ovarian surgery still persist, particularly regarding the best timing for these procedures and the most effective long-term surveillance strategies. While recommendations vary among different organisations, they typically suggest undertaking such surgeries after family planning has been completed.
Removing the ovaries induces surgical menopause, as the ovaries are the primary source of female hormones. The side effects of surgical menopause may include:
Although removing the ovaries and fallopian tubes significantly lowers the risk of ovarian cancer, the peritoneum remains susceptible to primary peritoneal cancer. This type of cancer occurs at a rate of approximately 2%-4% post-surgery and is also known as extra-ovarian serous carcinoma—a cancer affecting the lining cells of the peritoneum or abdominal cavity. Given that ovarian and peritoneal epithelia share a common embryonal origin, it's believed that these cells can develop into cancer in individuals with BRCA1 or BRCA2 mutations who are at higher risk.
While hysterectomy or oophorectomy does not entirely eliminate the risk of cancer recurrence, there are additional benefits beyond reducing the risk of ovarian cancer.
A study conducted with 483 women who have disease-associated germline BRCA1/2 mutations demonstrated a significant outcome in the prevention of breast cancer. The findings revealed that those who underwent preventive bilateral prophylactic oophorectomy experienced about a 50% reduction in their risk for breast cancer.
At OncoCare Cancer Centre, genetic counselling with our specialists is available if needed. Genetic testing is offered if there should be concerns that hereditary cancer risk exists in the family. The process of genetic counselling provides patients and their families with information on cancer risks, and the implication of genetic testing so as to work towards a prevention strategy for cancer.
“Expert knowledge means better care for cancer”
Written by:
Dr Peter Ang
MBBS (Singapore)
MMed (Int Med)
MRCP (UK)
FAMS (Medical Oncology)
Site Map | PDPA | Terms of Use | Disclaimer |
Contact Us | Career | Media Contact